Have you ever noticed how difficult it is to stick to healthy routines when you’re stressed, anxious, or overwhelmed? You’re not alone.
I’ve worked with hundreds of clients on their health upgrade journeys, and one of the most common challenges they face is incorporating new habits, especially when their nervous system is under pressure. It’s not a motivation issue. It’s a nervous system issue.
The more we understand how our biology influences our behavior, the more empowered we become to make lasting change. That’s where Polyvagal Theory comes in, a powerful framework developed by Dr. Stephen Porges that explains how our sense of safety directly impacts our ability to form and sustain routines.
Understanding Polyvagal Theory
The Polyvagal Theory offers a powerful lens for understanding how our bodies and brains respond to safety and threat. It shows that the autonomic nervous system doesn’t operate like a simple “on/off” switch between relaxed and stressed. Instead, it moves through three distinct states, each with its own physiological and behavioral responses.[1]
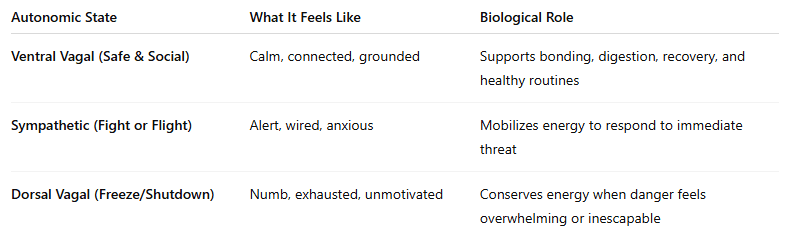
When we feel truly safe, physically, emotionally, and socially, the ventral vagal pathway, a branch of the parasympathetic nervous system, becomes active. This is the state where we feel capable of connection, creativity, and engaging in daily routines. The vagus nerve, the primary nerve of the parasympathetic system, sends calming signals to the brain and body, helping us rest, digest, and heal.[2]
When a threat is detected (like a looming deadline or a tense conversation), the body shifts into sympathetic activation, better known as “fight or flight.” Stress hormones like cortisol and adrenaline surge, sharpening our focus and vigilance. But over time, this state suppresses digestion, immune response, and emotional regulation.[3]
If the threat feels overwhelming or inescapable, the nervous system drops into the dorsal vagal state, a “freeze” response. Energy plummets. Motivation disappears. People often feel numb, shut down, or disconnected. It’s a biological form of self-protection, but it can derail the ability to stick to routines, even those meant to promote well-being.[4]
Understanding these states explains why routines fall apart under stress. It’s not about discipline, it’s biology. Once we learn how to shift back into a ventral vagal state, routines become not only possible, but sustainable.
Why Routines Slip in Times of Stress
Once you understand these autonomic states, it becomes clear why even the best intentions can unravel. When we’re stuck in fight-or-flight or freeze mode, the brain prioritizes short-term survival over long-term goals—like your morning walk or nightly wind-down routine.
I’ve seen this pattern time and again: clients are motivated to adopt healthier habits, but the moment stress ramps up, those routines collapse. It’s not because they’re unmotivated. It’s because their nervous system is doing its job, keeping them safe by shifting resources away from behaviors it doesn’t view as essential.[5]
How to Shift Back to a Regulated State
The good news is that the nervous system can be trained, and there are tools to help. One of the most exciting developments in recent years is the use of transcutaneous cervical vagus nerve stimulation (tcVNS). This is a non-invasive method that delivers gentle stimulation to the vagus nerve through the neck to promote parasympathetic (ventral vagal) activity.[6]
Devices like Truvaga use this technology to support relaxation, clarity, and better sleep in just two-minute sessions. Clinical studies have shown that VNS can improve:
- Heart rate variability (HRV) – an important marker of nervous system flexibility and resilience⁶
- Cognitive function and mood regulation[7]
- Stress response and emotional recovery after challenges[8]
These devices mimic the body’s own calming signals, helping users shift out of survival mode and into a more balanced state, one where healthy routines feel natural again.
Pairing VNS with Restorative Practices
In my practice, I’ve seen the best outcomes when vagus nerve stimulation is paired with simple, consistent rituals. These practices help send additional safety signals to the brain and deepen the benefits of VNS.
Mindfulness & Gratitude
- A few minutes of gratitude journaling
- Mindful breathing or grounding techniques
Breathing for Regulation
- Nasal, diaphragmatic breathing
- Box breathing (4-4-4-4) or 4-7-8 patterns
- Guided breathwork paired with Truvaga sessions
Vocal Vagus Exercises
- Humming, chanting, or singing
- Gargling (especially in the morning)
Bookend Your Day
- Morning: VNS + sunlight exposure + a calming intention
- Evening: VNS + reading a physical book + screens off before bed
These rituals, paired with vagus nerve stimulation, which I explore in my book “Upgrade Your Vagus Nerve,” help anchor your nervous system in the ventral vagal state, one of calm, creativity, and connection.
Make It Stick with Habit Stacking
One of the most effective ways to turn these tools into a lifestyle is habit stacking, the practice of pairing a new habit with an existing one.
For example:
After brushing your teeth in the morning, use your Truvaga device for two minutes and take five slow breaths.
This approach reduces decision fatigue, increases consistency, and helps rewire your nervous system over time.[9]
Final Thoughts: Build from Safety
Polyvagal Theory reminds us that our ability to change doesn’t come from willpower alone, it comes from how safe our body feels. Safety, as Dr. Porges reminds us, is not just the goal, it’s the foundation. When we start with the nervous system, everything else becomes easier.
So don’t start with discipline. Start with calm. One breath. One moment of gratitude. One two-minute session of vagus nerve stimulation. Small, intentional steps can reset your system and your routine.
Ready to feel calmer, clearer, and more connected?
Author bio:
Dr. Navaz Habib, is the bestselling author of “Activate Your Vagus Nerve,” and the newly released “Upgrade Your Vagus Nerve.” He is also the host of “The Health Upgrade Podcast.”
After graduating as class valedictorian from Canadian Memorial Chiropractic College in 2010 and went on to practice traditional chiropractic for years, until he utilized the power of functional medicine to transform his own health. Dr. Habib is the founder of “Health Upgraded” an online functional health consulting clinic, supporting optimal health by elevating the awareness and function of the vagus nerve.
References
- Porges, Stephen W. 1995. “Orienting in a defensive world: Mammalian modifications of our evolutionary heritage.” Psychophysiology 32(4):301–318. https://doi.org/10.1111/j.1469-8986.1995.tb01213.x
- Arnsten, Amy F.T. 2009. “Stress signalling pathways that impair prefrontal cortex structure and function.” Nature Reviews Neuroscience 10:410–422. https://doi.org/10.1038/nrn2648
- Burger, Andreas M. et al. 2020. “Effects of non-invasive vagus nerve stimulation on mental health.” Journal of Psychiatric Research 130:31–37. https://doi.org/10.1016/j.jpsychires.2020.07.024
- Clancy, J. A., et al. 2014. “Non-invasive vagus nerve stimulation in healthy humans reduces sympathetic nerve activity.” Brain Stimulation 7(6):871–877. https://doi.org/10.1016/j.brs.2014.07.031
- Clear, James. 2018. Atomic Habits: An Easy & Proven Way to Build Good Habits & Break Bad Ones. Avery. https://jamesclear.com/atomic-habits
- Brock C, Brock B, Aziz Q, Møller HJ, Pfeiffer Jensen M, Drewes AM, Farmer AD. Transcutaneous cervical vagal nerve stimulation modulates cardiac vagal tone and tumor necrosis factor-alpha. Neurogastroenterol Motil. 2017 May;29(5). doi: 10.1111/nmo.12999. Epub 2016 Dec 12. PMID: 27957782.
- McIntire LK, McKinley RA, Goodyear C, et al. Cervical transcutaneous vagal nerve stimulation (ctVNS) improves human cognitive performance under sleep deprivation stress. Commun Biol. 2021;4:624. doi:10.1038/s42003-021-02145-7
- Gurel NZ, Wittbrodt MT, Jung H, Shandhi MMH, Driggers EG, Ladd SL, Huang M, Ko YA, Shallenberger L, Beckwith J, Nye JA, Pearce BD, Vaccarino V, Shah AJ, Inan OT, Bremner JD. Transcutaneous cervical vagal nerve stimulation reduces sympathetic responses to stress in posttraumatic stress disorder: A double-blind, randomized, sham-controlled trial. Neurobiol Stress. 2020 Oct 20;13:100264. doi: 10.1016/j.ynstr.2020.100264. PMID: 33344717; PMCID: PMC7739181.
- Redwine, Lisa et al. 2016. “Gratitude journaling improves heart rate variability in patients with heart failure.” Psychosomatic Medicine 78(6):667–676. https://doi.org/10.1097/PSY.0000000000000322